Benefits of 3-D Mammograms Last Over Time
A study looking at 3 years of data on 3-D mammogram screening has found that the benefits of 3-D mammograms, including finding more cancers and reducing call-back rates, last over time.
Published on February 27, 2016
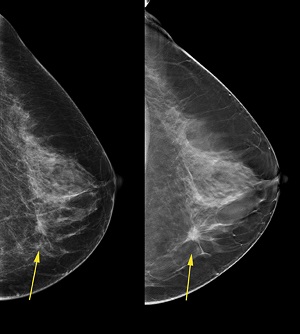
Three-dimensional mammography (also called digital breast tomosynthesis, digital tomosynthesis, or just tomosynthesis) creates a three-dimensional picture of the breast using X-rays. Several low-dose images from different angles around the breast are used to create the 3-D picture.
A conventional mammogram creates a two-dimensional image of the breast from two X-ray images of each breast.
Three-dimensional mammography is approved by the U.S. Food and Drug Administration, but isn’t yet considered the standard of care for breast cancer screening. Because it’s relatively new, it’s not available at all hospitals and mammogram facilities.
Still, 3-D mammography technology seems to be being adopted faster throughout the United States than digital mammography was -- 50% of the facilities in the Breast Cancer Surveillance Consortium now offer 3-D mammograms. The Breast Cancer Surveillance Consortium is a collaborative network of seven mammography registries with linkages to tumor and/or pathology registries. The network is part of the National Cancer Institute.
Several studies have found that 3-D mammograms find more cancers than traditional 2-D mammograms and also reduce the number of false positives. Still, these studies didn’t look at 3-D mammogram screening over time.
A false positive is when a mammogram shows an abnormal area that looks like a cancer but turns out to be normal. Ultimately, the news is good: no breast cancer. But the suspicious area usually requires follow-up with more than one doctor, extra tests, and extra procedures, including a possible biopsy. There are psychological, physical, and economic costs that come with a false positive.
The rate of false positives has helped fuel the ongoing debate about the value of screening mammograms.
A study looking at 3 years of data on breast cancer screening with 3-D mammograms has found that the benefits of 3-D mammograms last over time.
The study was published online on Feb. 18, 2016 by JAMA Oncology. Read the abstract of “Effectiveness of Digital Breast Tomosynthesis Compared With Digital Mammography: Outcomes Analysis From 3 Years of Breast Cancer Screening.”
"These findings reaffirm that 3-D mammography is a better mammogram for breast cancer screening," said Emily Conant, M.D., chief of breast imaging at the Perelman School of Medicine at the University of Pennsylvania, who was the senior author of the study. Dr. Conant also is a member of the Breastcancer.org Professional Advisory Board. "These results are an important step toward informing policies so that all women can receive 3-D mammography for screening."
In the study, the researchers analyzed 44,468 screening mammograms of 23,958 women who had never been diagnosed with breast cancer. From September 2010 to August 2011, all the women were screened with digital 2-D mammograms only. For the next 3 years, the women were screened with 3-D mammograms.
The researchers compared differences in screening outcomes between each 3-D mammogram year and the 2-D digital mammogram year. They also compared the differences in outcomes between women who had one, two, or three 3-D mammograms.
The rates of women who had to come back for more testing increased slightly each year for women who had 3-D mammograms:
- year one recall rate: 88 per 1,000 women screened
- year two recall rate: 90 per 1,000 women screened
- year three recall rate: 92 per 1,000 women screened
Still, these rates were much lower than the recall rate of 104 per 1,000 women screened for 2-D mammograms. This difference was statistically significant, which means that it was likely because of the difference in screening technique rather than just due to chance.
The rate of cancers found in women who were called back for more testing went up in women who had 3-D mammograms compared to women who had 2-D mammograms -- meaning that 3-D mammograms found more cancers than 2-D mammograms. Rates of cancer detection in women who were called back for more testing were:
- 4.4% in women who had 2-D mammograms
- 6.2% in year one of 3-D mammograms
- 6.5% in year two of 3-D mammograms
- 6.7% in year three of 3-D mammograms
When the researchers compared recall rates between women who had one, two, or three 3-D mammograms, they found that these rates went down as women had more 3-D mammograms. Recall rates were:
- 130 per 1,000 women screened for women who had one 3-D mammogram
- 78 per 1,000 women screened for women who had two 3-D mammograms
- 59 per 1,000 women screened for women who had three 3-D mammograms
Interval cancers are cancers that are found within 12 months after a normal mammogram. Rates of interval cancers went down slightly from 0.7 per 1,000 women screened with 2-D mammograms to 0.5 per 1,000 women screened with 3-D mammograms.
The authors said that the study provides the first longitudinal evidence that the benefits of initial 3-D mammogram screening can be sustained and improved over time with consecutive 3-D mammogram screening.
These results are very exciting and may help 3-D mammography become part of routine breast cancer screening.
To learn more about 3-D mammography, including how it’s done and how it’s different from 2-D mammography, visit the Breastcancer.org Digital Tomosynthesis page.
Share your feedback
Help us learn how we can improve our research news coverage.
Was this article helpful?