Invasive Ductal Carcinoma (IDC)
Updated on December 5, 2024
What is invasive ductal carcinoma?
Invasive ductal carcinoma (IDC), also called infiltrating ductal carcinoma, is the most common type of breast cancer. About 80% of all breast cancers are IDC, according to the American Cancer Society.
Invasive means the cancer has spread into surrounding breast tissues. Ductal means the cancer started in the milk ducts, the tubes that carry milk from the lobules to the nipple. Carcinoma refers to any cancer that begins in the skin or other tissues that cover the lining of internal organs, such as breast tissue.
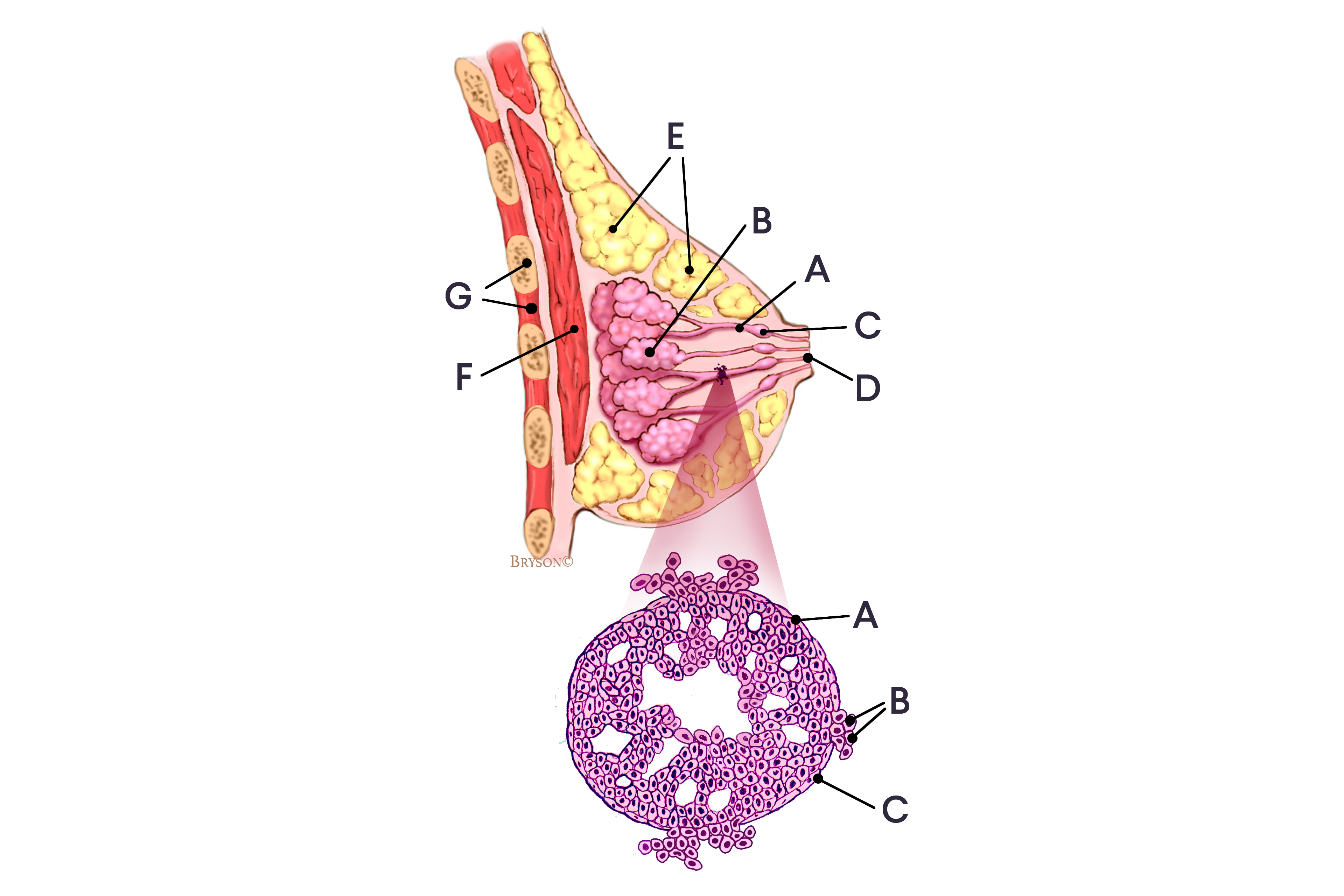
Normal breast with invasive ductal carcinoma (IDC) in an enlarged cross-section of the duct
Breast profile: A Ducts B Lobules C Dilated section of duct to hold milk D Nipple E Fat F Pectoralis major muscle G Chest wall/rib cage
Enlargement: A Normal duct cell B Ductal cancer cells breaking through the basement membrane C Basement membrane
Signs and symptoms of invasive ductal carcinoma
In many cases, invasive ductal carcinoma causes no symptoms and is found after your doctor sees a suspicious area on a screening mammogram.
In other cases, you or your doctor may feel a lump or mass in your breast. Other signs of invasive ductal carcinoma include:
swelling of all or part of the breast
skin irritation
skin dimpling, sometimes looking like an orange peel
breast or nipple pain
nipple turning inward (retraction)
nipple discharge, other than breast milk
redness, scaliness, or thickening of the nipple or breast skin
a lump or swelling in the underarm area
Diagnosis of invasive ductal carcinoma
Diagnosing invasive ductal carcinoma involves a combination of procedures and almost always includes:
Other tests that may be used are:
Staging invasive ductal carcinoma
The stage of invasive ductal carcinoma is determined by the cancer’s characteristics, such as how large it is and whether or not it has hormone receptors. The stage of the cancer helps you and your doctor:
decide on the best treatment options for you
determine if certain clinical trials may be a good option for you
figure out your prognosis
Generally, the stage of invasive ductal carcinoma is described as a number on a scale of I through IV.
stages I, II, and III describe early-stage cancers that have not spread outside the breast or the lymph nodes in the underarm on the same side as the breast cancer
stage IV describes cancers that have spread outside the breast and underarm lymph nodes to other parts of the body, such as the bones or liver
Grades of invasive ductal carcinoma
The cancer grade, also called the Nottingham grade or histologic score, can vary from low to high. A cancer’s grade is based on how much cancer cells look like normal cells. Cancer grade is different from cancer stage. There are three cancer grades:
Grade 1, or low grade, usually refers to cancer that grows slowly and is less likely to spread.
Grade 2, or moderate grade, refers to cancer that is growing faster than a grade 1 but slower than a grade 3.
Grade 3, or high grade, refers to cancer that is growing faster than grade 1 and grade 2 and which is more likely to spread.
Typically, cancer that has a low grade has better treatment outcomes.
If you have been diagnosed with invasive ductal carcinoma, your doctor will do more tests to collect information on the cancer’s characteristics. These tests, as well as the results of your biopsy, make up the parts of your pathology report.
Information commonly collected as part of a pathology report includes:
size of the breast cancer
tumor necrosis
lymphovascular invasion
rate of cell growth (Ki-67 levels)
Treatment for invasive ductal carcinoma
Treatments for invasive ductal carcinoma may include:
Surgery: You and your doctor work together to determine the type of surgery that’s right for you, based on the cancer’s characteristics, your family and medical history, and your preferences.
Radiation therapy: Radiation therapy is almost always recommended after lumpectomy and may be recommended after mastectomy if the cancer is large or if cancer is found in the lymph nodes.
Chemotherapy: Chemotherapy may be given before or after surgery. Your doctor takes the cancer’s characteristics and your medical history into consideration when deciding if chemotherapy is right for your unique situation.
Hormonal therapy: If the breast cancer has receptors for the hormones estrogen, progesterone, or both, your doctor is likely to recommend hormonal therapy, which is also called anti-estrogen therapy or endocrine therapy. Hormonal therapy medicines work by lowering the amount of estrogen in the body or by blocking the action of estrogen on breast cancer cells.
Targeted therapy: Targeted cancer therapies are treatments that target specific characteristics of cancer cells, such as a protein that allows the cancer cells to grow in a rapid or abnormal way. Some targeted therapies are antibodies. Antibodies are proteins made naturally by your immune system that find and attack foreign invaders, such as germs that cause infection. These types of targeted therapies work just like the antibodies made naturally by your immune system, and are sometimes called immune targeted therapies.
Immunotherapy: Immunotherapy medicines use your body’s immune system to attack cancer cells. The cancer’s characteristics determine if immunotherapy is a treatment option for you.
Follow-up care after invasive ductal carcinoma treatment
Because of better diagnostic tests and advances in cancer treatments, more people are living longer than ever after being diagnosed with any type of cancer, including breast cancer. Experts estimate that there are more than 4 million breast cancer survivors in the United States.
Still, because of treatments they’ve received, many breast cancer survivors have a higher risk of developing other diseases as they age, including high blood pressure, heart disease, and osteoporosis. If you’ve completed treatment for invasive ductal carcinoma, it’s important you get good follow-up care.
Your doctor can work with you to create a follow-up care plan that involves regular checkups so they can monitor your overall health, side effects of treatment, and more. Follow-up care plans may include:
the tests you need
which doctors order the tests
a schedule of when you need to have the tests
healthy living recommendations
resources, if you need more information
Subtypes of invasive ductal carcinoma
There are several rare subtypes of invasive ductal carcinoma. These are often named for features seen when the cells are looked at under a microscope, such as the way the cells are arranged. The symptoms, diagnosis, staging, treatment options, and follow-up care are generally the same for all IDC subtypes.
Tubular carcinomas of the breast
Tubular carcinomas account for less than 2% of all breast cancers. When looked at under a microscope, the cells of a tubular carcinoma look like tubes. These tumors tend to be low-grade. Tubular carcinomas are usually hormone receptor-positive and HER2-negative.
Medullary carcinomas of the breast
Medullary carcinomas account for less than 5% of all breast cancers. It is called “medullary” carcinoma because the tumor is a soft, fleshy mass that resembles a part of the brain called the medulla. Medullary carcinomas are often triple-negative {estrogen receptor-negative, progesterone receptor-negative, and HER2-negative}. But unlike most triple-negative breast cancers, which tend to be more aggressive, medullary carcinoma doesn’t grow quickly and usually doesn’t spread outside the breast to the lymph nodes.
Mucinous carcinomas of the breast
Mucinous carcinomas — also called colloid carcinomas — account for less than 2% of all breast cancers. It’s called “mucinous” carcinoma because the cancer produces mucin, a natural substance and key ingredient in mucus. Mucinous carcinomas are usually low-grade, and usually don’t spread outside the breast to the lymph nodes. Mucinous carcinomas are usually hormone receptor-positive and HER2-negative.
Papillary carcinomas of the breast
Papillary carcinomas of the breast account for less than 1% of all breast cancers. When the cells are looked at under a microscope, they have finger-like projections or “papules.” Papillary carcinomas are usually small, hormone receptor-positive, and HER2-negative.
Cribriform carcinomas of the breast
Cribriform carcinomas account for less than 1% of all breast cancers. In invasive cribriform carcinoma, the cancer cells invade the stroma (connective tissues of the breast) in nestlike formations between the ducts and lobules. Within the tumor, there are distinctive holes in between the cancer cells, making it look something like Swiss cheese. Invasive cribriform carcinoma is usually low grade.
Metaplastic carcinomas of the breast
Metaplastic carcinomas account for less than 1% of all breast cancers. Metaplastic breast cancers contain abnormal ductal cells, but also contain cells that look like the soft tissue and connective tissue in the breast. The ductal cells have changed their form to become completely different cells, though it’s not clear how or why this happens. When cells change form it’s called metaplasia, which gives this type of breast cancer its name. Metaplastic breast cancer is considered more aggressive and is usually high grade and triple-negative.
You can connect with others with a diagnosis of invasive ductal carcinoma by joining the IDC forum in the Breastcancer.org Community.