Having Kids After Breast Cancer Isn’t Simple: 4 Women Share Their Stories
Updated on October 2, 2025
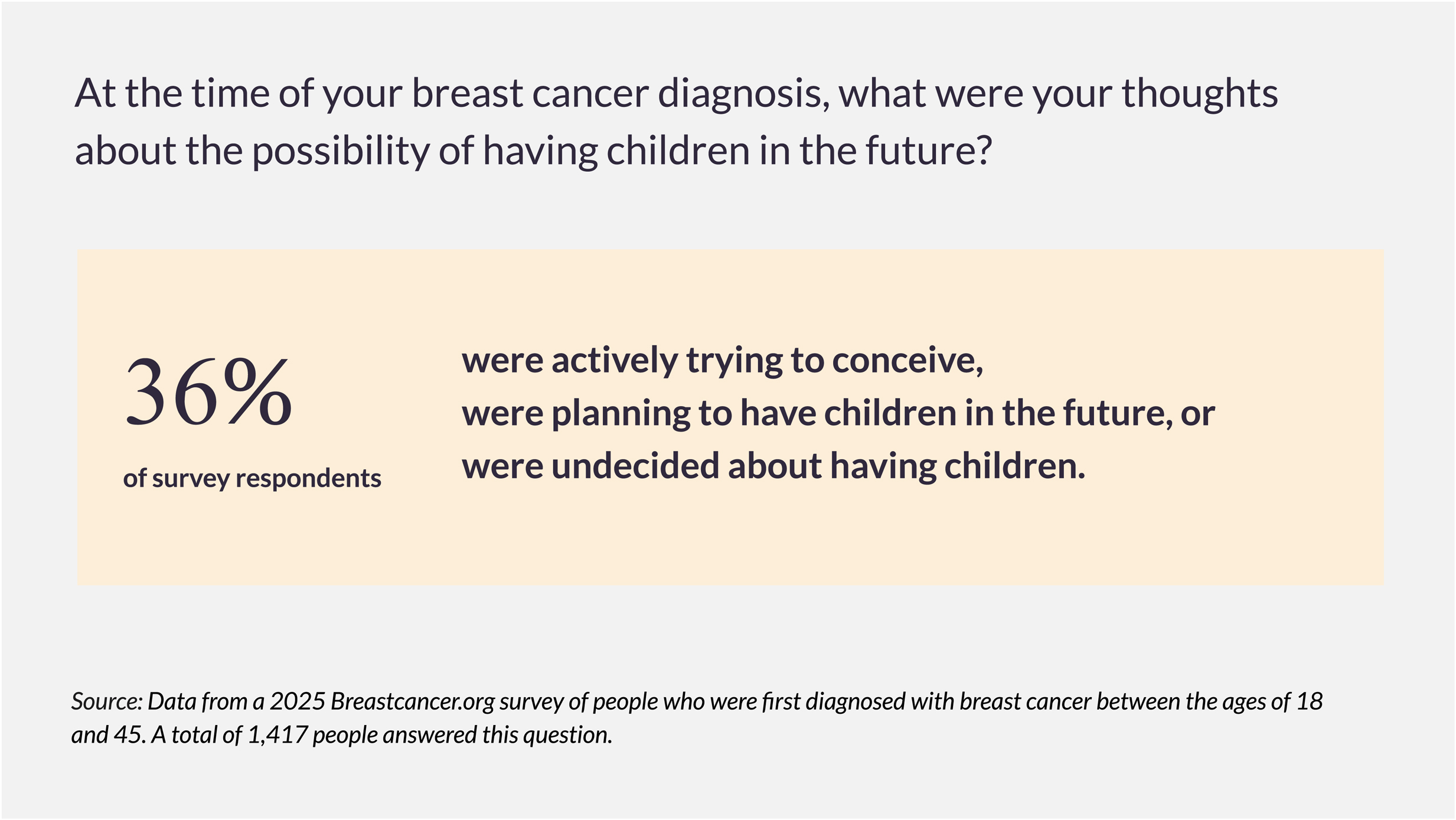
There are many more options today for people who want to have kids after breast cancer than there were even 10 years ago. It's still true that some breast cancer treatments can damage your fertility or cause permanent infertility. But fertility preservation procedures, done before treatment, are now more effective and widely available than they've ever been. More research about fertility after breast cancer has led to more options for pausing hormonal therapy to get pregnant or taking medicines during chemo that may help protect fertility.
“I’m seeing more women treated for breast cancer in my community and nationwide who are being offered support for preserving fertility,” says Virginia (Ginger) Borges, MD, MMSc, professor of medicine-medical oncology at the University of Colorado Anschutz Medical Campus in Aurora, Colorado.
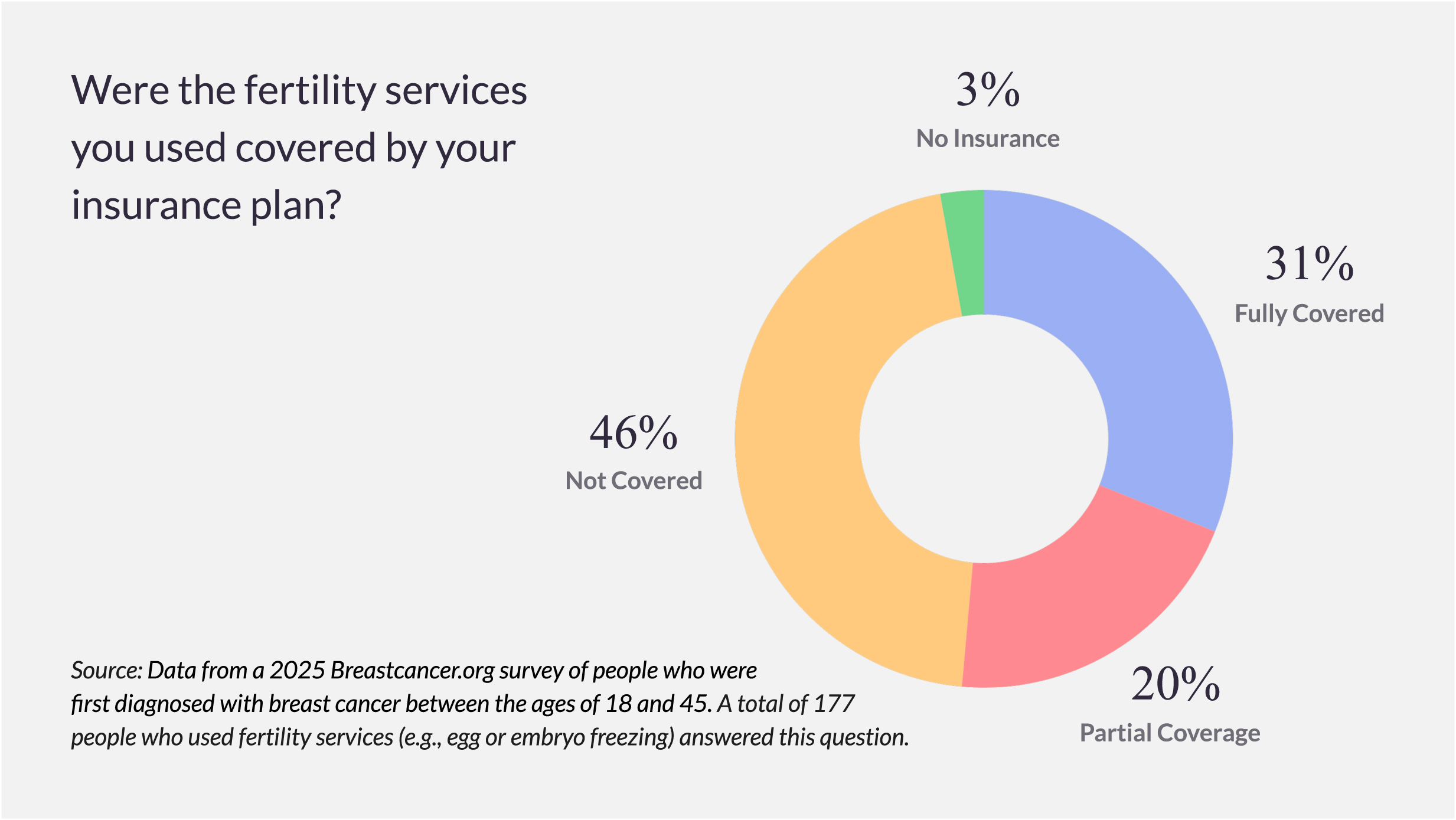
Even with these advancements, though, people who want to have a biological child after treatment often face complicated physical, emotional, financial, and logistical hurdles. The timing of treatments can dictate when they’re able to try to have a child and in some cases leave them with smaller windows of time than they ever expected. In some cases, they’re not receiving enough support from their medical team to navigate fertility decisions or fertility procedures and services are out of reach because they’re too expensive.
We spoke with four women who were diagnosed with breast cancer at a young age and hoped to have a biological child about how they looked into their options, managed uncertainties, and made difficult decisions.
Pausing hormonal therapy to try to get pregnant: Caitlin’s story
Three days after her wedding, Caitlin Perillo found a lump in her breast that turned out to be stage I invasive ductal carcinoma. She was 37 years old. Prior to her diagnosis, Perillo and her husband thought they would explore having children, but weren’t sure of their timeline. “My diagnosis forced us to make decisions in a very short period of time. You realize some options might be completely off the table if you don’t decide quickly,” Perillo says.
"Fifteen years from now, would we regret it if we didn’t take this path of trying to have children?”
Biggest decision: After Perillo had a mastectomy, she and her husband did one round of egg retrieval and attempted in vitro fertilization (IVF), which didn’t produce a viable embryo. “That was more gut-wrenching than we expected,” she says. “We didn’t realize we were so emotionally invested at that stage.”
Her oncologist recommended she not wait too long to start taking tamoxifen. Perillo and her husband initially didn’t know if they wanted to continue with IVF. “The process is physically and mentally taxing to go through while you’re also dealing with the roller coaster of the cancer diagnosis,” she says, “and it becomes even more stressful when you don't have the luxury of time.”
They decided to do a second round of IVF, and — after 18 months on tamoxifen — Perillo paused the treatment for the embryo transfer procedure. It was successful and Perillo gave birth to identical twin girls. “It was amazing that all of it came together,” Perillo says. “We spent the whole process holding our breath.”
On the financial ramifications: “IVF is not a cheap process. Our insurance covered most of the first round, but the second round had to be completely covered by us. We did ask ourselves: how much can we spend to potentially end up with children or not end up with children, since there’s no guarantee? We had a lot of bills coming from my cancer treatment and it’s not like we’re sitting on a pile of cash.”
Tips for others in similar situations: “Give yourself the space you need to make decisions, even though your doctors make you feel like the clock is ticking. If you have a partner, have open conversations with them in which both of you can share your concerns and feelings. It’s hard to think about fertility when you’re already mentally and physically drained because of the cancer diagnosis, but it was helpful for us to stop and ask ourselves: ‘Fifteen years from now, would we regret it if we didn’t take this path of trying to have children?’”
Choosing surrogacy after infertility: Rachael’s story
When Racheal Liebert was diagnosed with early-stage, triple-negative breast cancer at the age of 34, she had a 2-year-old son and hoped to have another child. She talked with her doctors about doing fertility preservation procedures before starting treatment, but because of the aggressive nature of her diagnosis, she was eager to start chemotherapy. “But having a second child was still always on my mind,” Liebert says.
Biggest decision: Liebert has a BRCA1 gene mutation, which raises the risk of ovarian cancer. So she decided, based on the recommendation of her doctors, to have her ovaries, fallopian tubes, and uterus removed as part of her treatment. Liebert and her husband began exploring adoption and surrogacy and, after a lot of research, decided to move forward with a surrogacy agency. Five years after Liebert’s diagnosis, they welcomed their second child, a son. “My surrogate was so supportive and kind throughout the process. I remain very close to her and plan to for many years to come,” says Liebert.
On secondary infertility after breast cancer: “You already have the joy of being a parent, but because of cancer you may not get to have the family you envisioned. It can be isolating and it deserves more attention. Some of my very close friends who had supported me during my treatment were surprised when I opened up to them about the sadness of potentially not being able to have a second child.”
Tips for others in similar situations: “If you’re interested in surrogacy, talk with people who have had children that way and meet with a few different surrogacy agencies to get a sense of what they’re like. Surrogacy is a long, complicated, emotionally intense, and very expensive process, so it’s important to understand your options. I also recommend seeing if your employer and your partner’s employer (if you have a partner) has a program that provides financial support to employees that are pursuing surrogacy or adoption. My husband’s employer covered a small portion of our surrogacy costs, which was helpful.”
Read more of our series on being diagnosed young with breast cancer, and learn about how giving birth can raise the risk of developing more aggressive breast cancers.
Not getting the chance to do fertility preservation: Vicki’s story
In the year leading up to her breast cancer diagnosis, Vicki Gonzalez had been trying to have her first child and had experienced two devastating pregnancy losses. When she found out that she had early-stage, hormone receptor-positive invasive ductal carcinoma, her biggest immediate concern was her fertility. She felt that she and her husband had a dwindling window to have a biological child because she was 40 years old. “I was particularly worried about what chemo would do to my fertility,” Gonzalez says, “and I brought that up to my treatment team multiple times.”
Biggest regret: Gonzalez didn’t freeze her eggs before starting chemo, a decision that she deeply regrets. When she had asked her oncologist about it, he had said that freezing her eggs could delay the start of her treatment by months — which wasn’t actually true — and he didn’t bring up the possibility of referring her to a fertility specialist for a consultation. Instead, he presented her with a plan: After her active treatment ended, she could delay starting tamoxifen to try to get pregnant naturally. That didn’t work out, though. Since Gonzalez finished active treatment, she has been in chemically induced menopause, and an ultrasound of her ovaries didn’t show any signs that she would start menstruating or ovulating again anytime soon. She is currently taking tamoxifen and Verzenio, and has given up for now on trying to get pregnant.
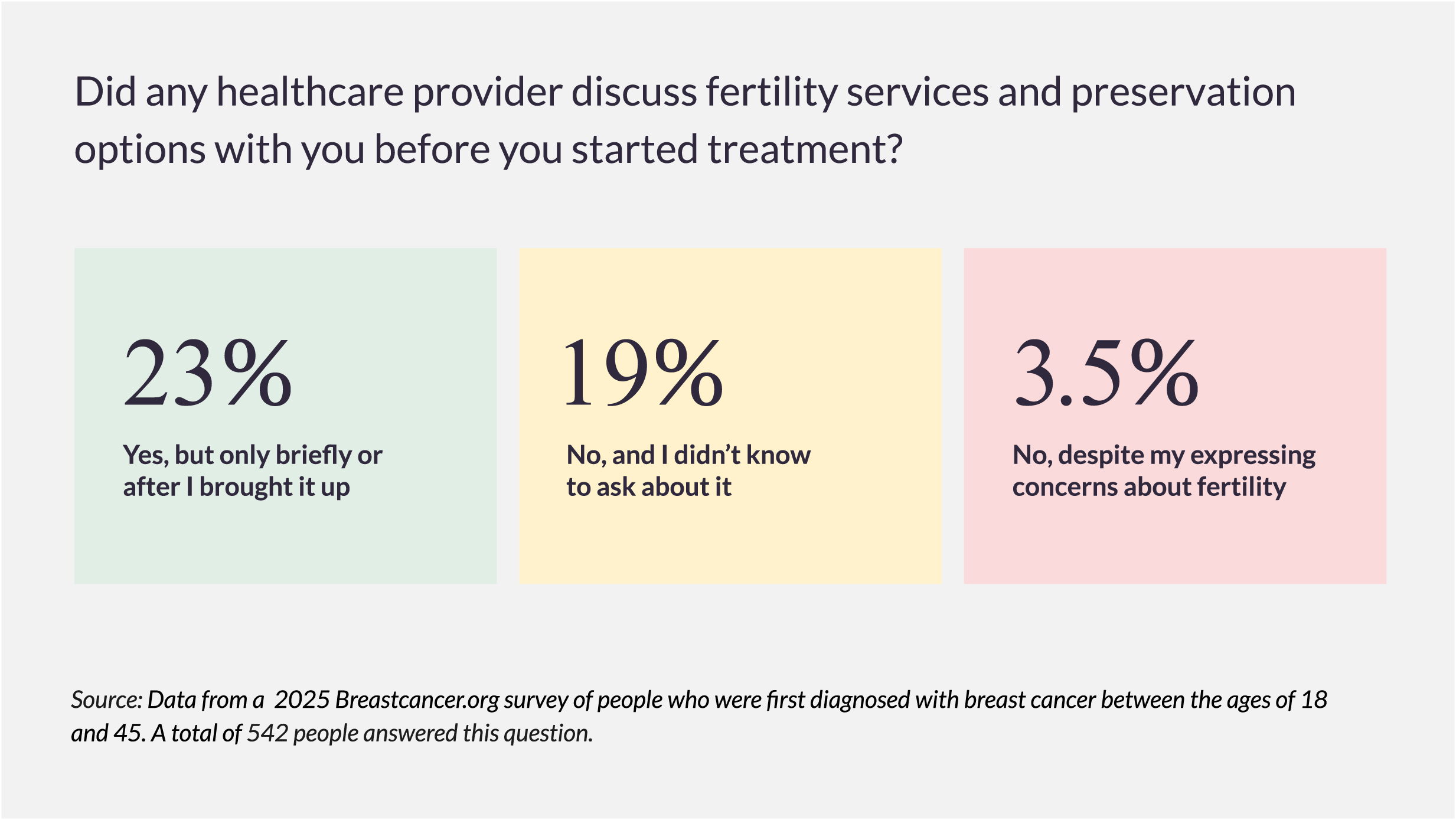
On trusting her oncologist’s advice too much: “I took what my oncologist had told me at face value because I was in a vulnerable situation and feeling really overwhelmed,” Vicki says. “Later I found out that I could have had more options.”
Tips for others in similar situations: “Always ask to be referred to a fertility specialist, so you can at least find out what all your options might be for fertility preservation. No one in my cancer treatment team gave me any navigation about fertility before treatment started. I even took a class on chemo at the hospital, and fertility wasn’t mentioned at all.
“Also, look into whether your state has laws requiring some types of insurance plans to cover fertility preservation procedures for people undergoing cancer treatments that could cause infertility. I found out too late that my state has a law like that. I wasn’t financially prepared to pay for fertility preservation out of pocket. But no one told me about that law before my treatment started, when I could have benefitted from it.”
Making the hard decision not to have another child: Jessica’s story
Six months after giving birth to her son, Jessica Matfus learned that a lump she had thought was a clogged milk duct was actually stage II, triple-negative breast cancer. She was 32 years old and wanted to eventually have more children. “Coming from a big family, I always thought that I’d have at least three kids,” Matfus says. So her oncologist recommended that she do a round of IVF before starting chemo and having surgery. She and her husband wound up with several embryos that would be frozen and stored until they decided when, or if, to use them.
On what it was like to undergo IVF while caring for a baby and preparing for treatment: “I had a lot of mixed emotions about it. I didn’t have enough time to think through the decision. I wish I could go back and tell myself then: ‘Don’t do it — you will be happy with one child. It’s not worth the extra layer of stress and pumping hormones into your body, given everything else you’re dealing with.’ But at the time, it almost felt like I didn’t have a choice…it was what I had to do to avoid potential future regret.”
Biggest decision: Matfus and her husband took several years to decide whether to try to have a second child using their frozen embryos. Ultimately, they opted not to.
While Matfus’s doctors thought it was safe enough for her to try to get pregnant, they also acknowledged that it wasn’t clear if, or how much, it would raise her risk of recurrence, given her history. Because of this, Matfus didn’t feel comfortable with the idea of carrying a child herself, and she didn’t feel that other options, like surrogacy, were the right fit. “It will always be a difficult decision. It took a lot of time, thought, and therapy,” she says. “But I’m happy with the way my family turned out.”
Tips for others in similar situations: “Make your mental health a priority. Talk with other survivor friends, join support groups, and find a good therapist who specializes in [working with] people with cancer. Taking care of your mental wellness will really prevent you from being isolated and feeling like you can’t move on with your life post-treatment. I got really lucky that I did find support.”
This content is made possible, in part, by Novartis and Lilly.


