Breast Self-Exam: Get to Know Your Breasts in 5 Steps
Updated on September 30, 2025
Doing a breast self-exam means checking your breasts, by sight and by touch, for any changes, like a new lump.
While most medical organizations no longer recommend formal breast self-exams, experts agree that becoming familiar with how your breasts normally look and feel is essential.
“What really matters most is to understand the baseline of what’s normal for you, so you can notice any breast changes early on,” says Mediget Teshome, MD, FACS, MPH, chief of breast surgery and director of breast health at UCLA Health in Los Angeles. “If a new change — like skin dimpling, nipple inversion, or a breast lump — persists rather than going away, then you should talk with your doctor about it.”
Breast self-exam guidelines
Through the years, there has been some debate among medical experts about how valuable formal breast self-examination is in finding breast cancer early and increasing the chances of survival. Studies have shown that regular breast self-examination doesn’t have a meaningful effect on breast cancer survival rates and may even cause harm by resulting in unnecessary biopsies.
Because of this, the American Cancer Society stopped recommending breast self-exam as a screening tool for women with an average risk of breast cancer. Other medical organizations that issue breast cancer screening recommendations — such as the U.S. Preventive Services Task Force and the American College of Obstetricians and Gynecologists — also don’t recommend breast self-exams.
Some experts recommend that people focus on “breast self-awareness” rather than on doing formal, step-by-step breast self-exams on a regular basis. Breast self-awareness means becoming familiar with how your breasts normally look and feel, so you’ll be more likely to notice any changes.
Others argue that detailed, step-by-step breast self-exams are worthwhile since they’re a convenient, no-cost tool you can use at any age as part of your overall breast cancer screening strategy. Plus, many people report that finding a lump on their own at home was what led to a diagnosis of breast cancer. Studies have shown that about 25% or more breast cancers are first found this way.
Breast self-exam and breast cancer screening
Keep in mind that breast self-exam/self-awareness is not a substitute for other breast cancer screening methods. Some breast cancers cannot be detected by breast self-exam because they are too small. Self-exam should always be used along with:
regular physical exams by a doctor
ultrasound, MRI (magnetic resonance imaging), or both, when needed
Each of these screening tools works in a different way and provides your doctor with different information; together, they can offer a fuller picture of any breast changes.
Talk with your healthcare provider about developing a breast cancer screening strategy that makes sense for your unique situation and any individual risk factors. Ask your provider to do a breast cancer risk assessment, if you haven’t had one already. The American College of Radiology recommends that all women be evaluated by a doctor to find out if they’re at higher-than-average risk for breast cancer no later than age 25.
How to do a breast self-exam: Five steps for checking for breast cancer at home
While it's not necessary to do a formal, five-step breast exam to practice breast self-awareness, it can be an easy way to make sure you're covering all the bases.
"Some women may prefer to do something more routine and be very intentional about it," explains Dr. Teshome. "If that’s their way of having breast self-awareness, there's nothing wrong with that at all. But it might not be for everyone."
These steps are for the traditional, formal breast self-exam. You can use these as a jumping-off point to find a way to check your breasts that feels right for you.
Step 1: Examine your breasts in a mirror with hands on hips
Begin by looking at your breasts in the mirror with your shoulders straight and your arms on your hips.
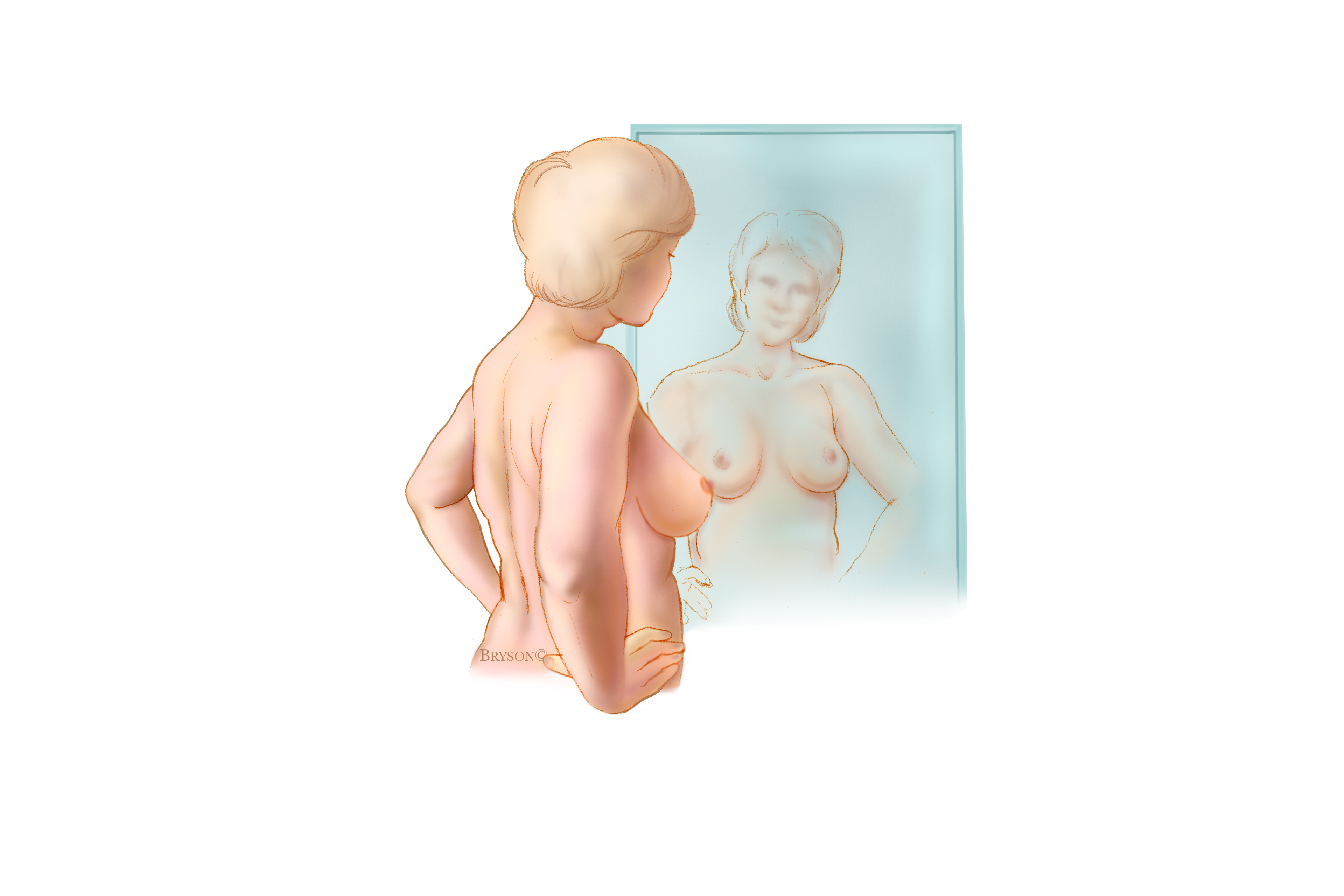
Here’s what you should look for:
breasts that are their usual size, shape, and color
breasts that are evenly shaped without visible distortion or swelling
If you see any of the following changes, bring them to your doctor’s attention:
dimpling, puckering, or bulging of the skin
a nipple that has changed position or an inverted nipple (pushed inward instead of sticking out)
redness, soreness, rash, or swelling
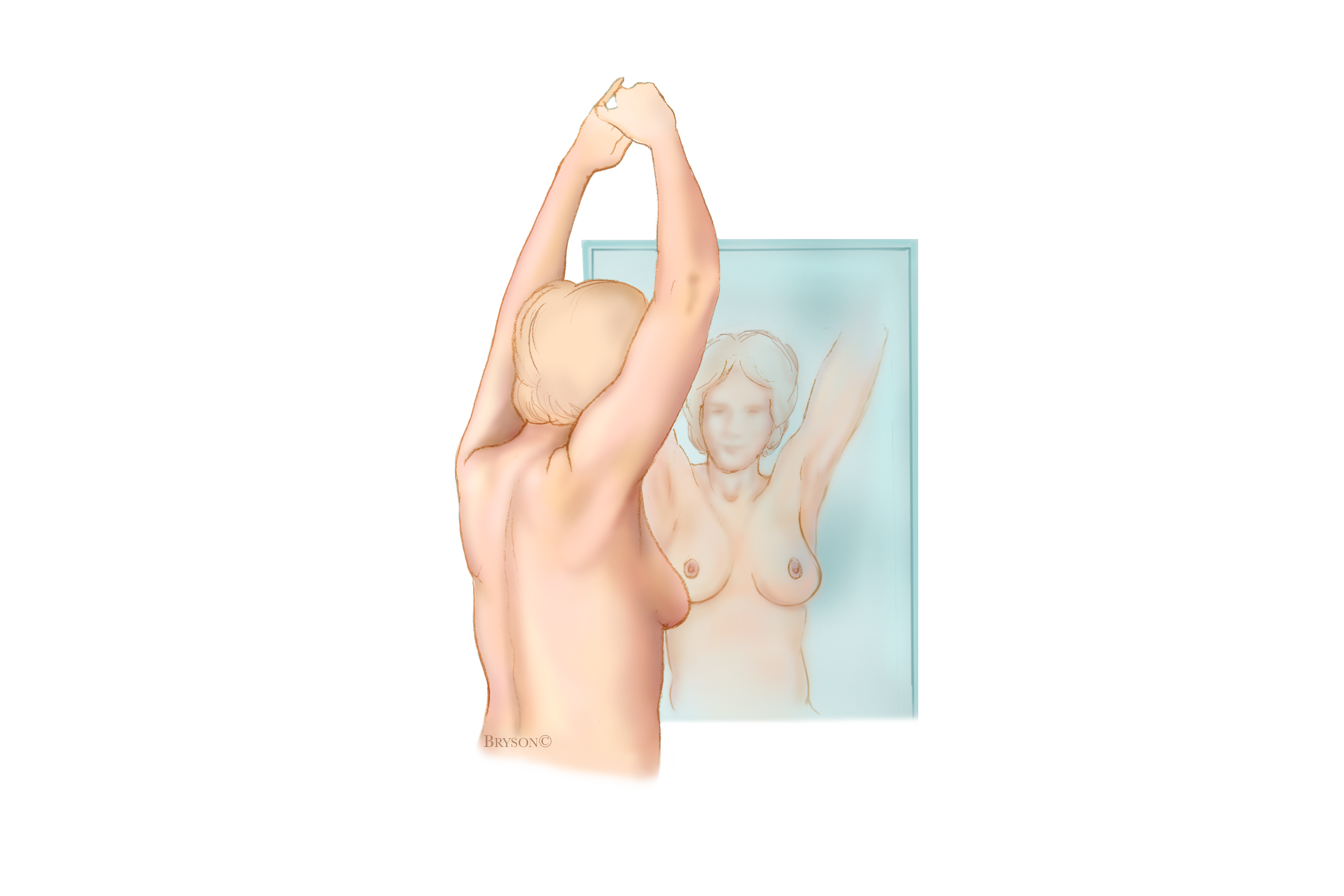
Step 2: Raise arms and examine your breasts
Now, raise your arms and look for the same changes.
Step 3: Look for signs of breast fluid
While you’re at the mirror, look for any signs of fluid coming out of one or both nipples (this could be a watery, milky, or yellow fluid or blood).
Step 4: Feel for breast lumps while lying down
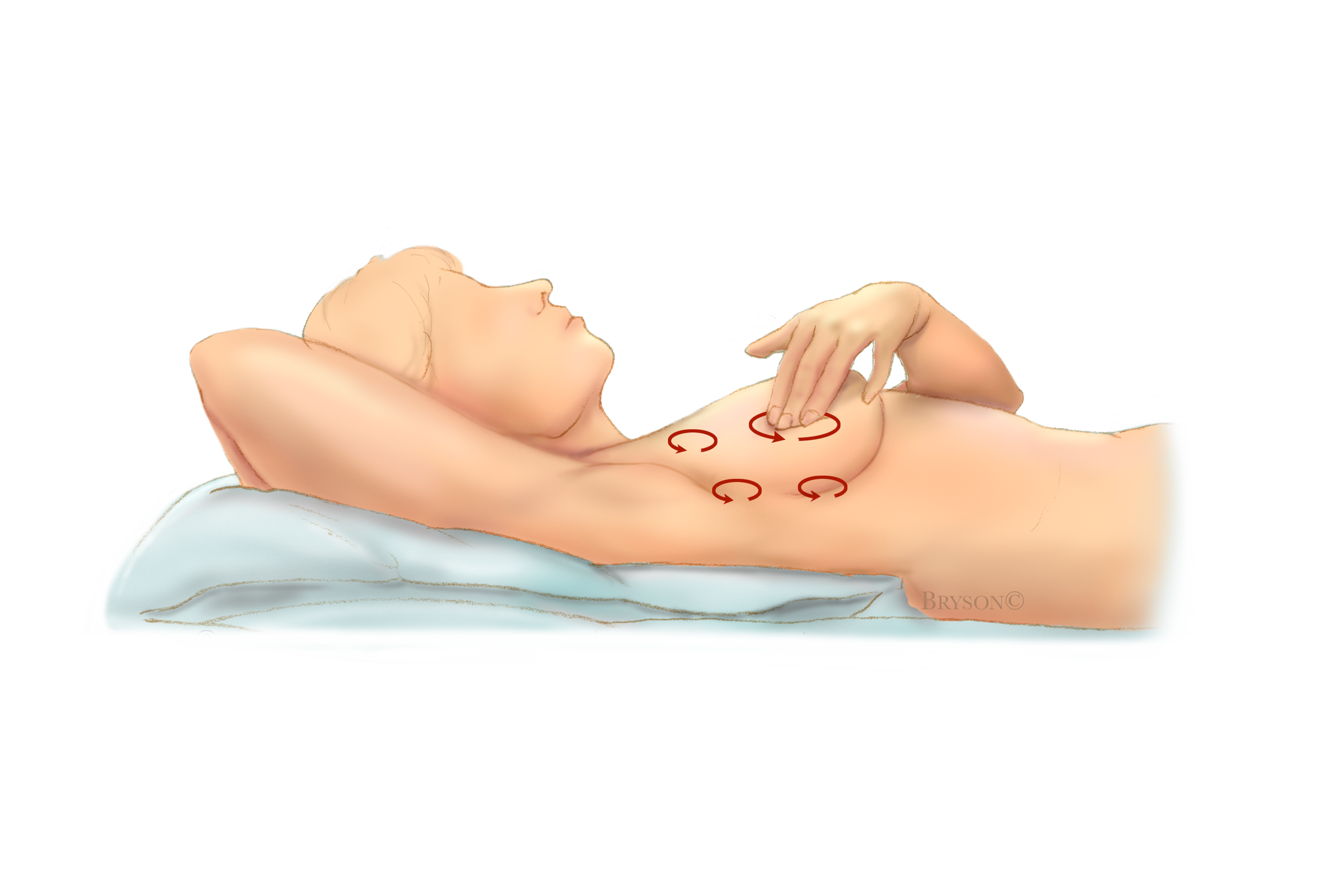
Next, check for breast lumps or abnormalities by feeling your breasts while lying down, using your right hand to feel your left breast, and then your left hand to feel your right breast. Use a firm, smooth touch with the first few finger pads of your hand, keeping the fingers flat and together. Press down with your fingers and move them in a circular motion that’s about the size of a quarter (or an inch around).
Cover the entire breast from top to bottom, side to side — from your collarbone to the top of your abdomen, and from your armpit to your cleavage.
Follow a pattern to be sure that you cover the whole breast. You can begin at the nipple, moving in larger and larger circles until you reach the outer edge of the breast. You can also move your fingers up and down vertically, in rows, as if you were mowing a lawn.
Be sure to feel all the tissue from the front to the back of your breasts. For the skin and tissue just beneath, use light pressure; use medium pressure for tissue in the middle of your breasts; use firm pressure for the deep tissue in the back. When you've reached the deep tissue, you should be able to feel down to your ribcage.
Step 5: Feel your breasts for lumps while standing or sitting
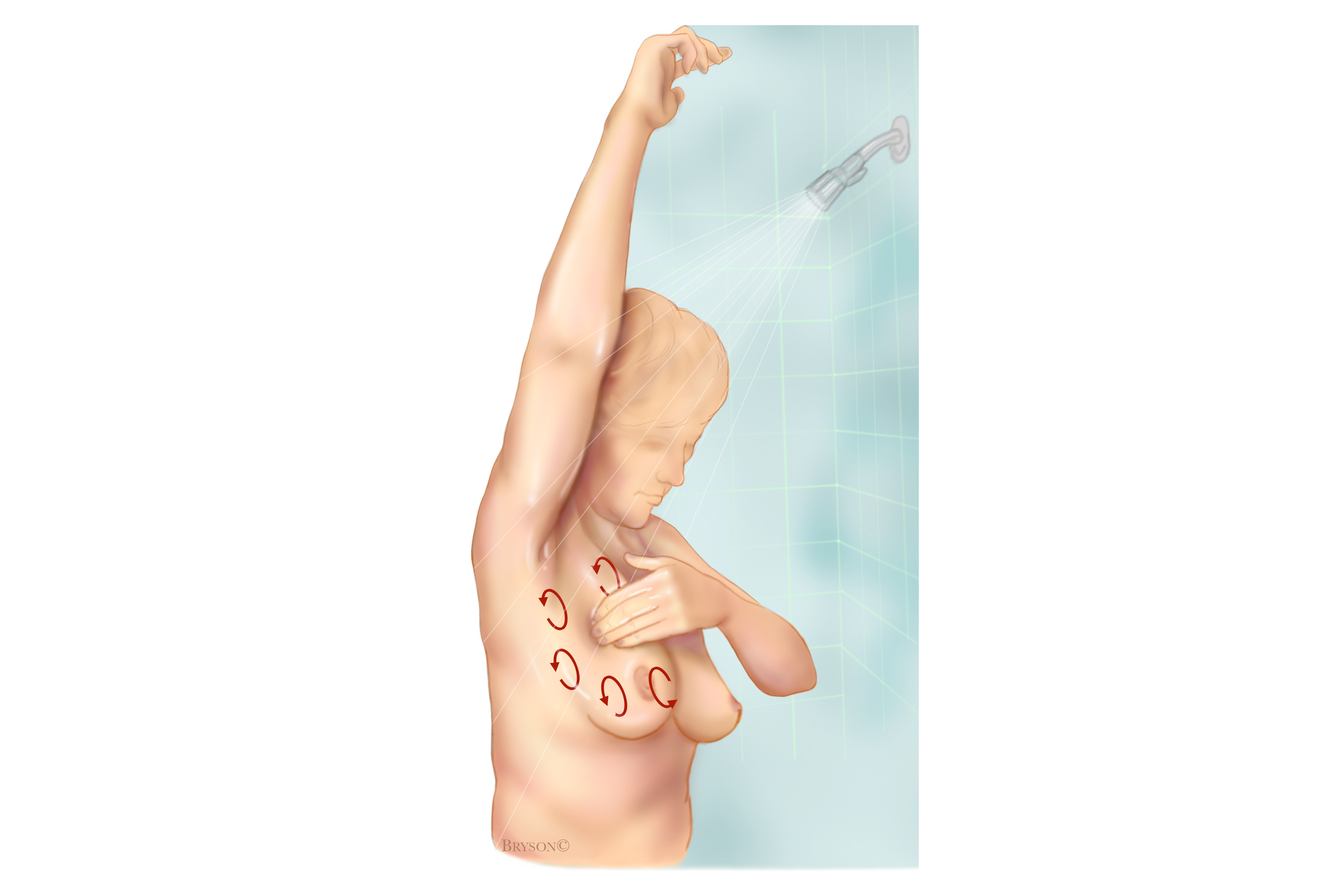
Finally, feel your breasts while you are standing or sitting. Many women find that the easiest way to feel their breasts is when their skin is wet and slippery, so they like to do this step in the shower. Cover your entire breast, using the same hand movements described in Step 4.
What should you do if you find a breast lump or other change?
Don’t panic
Most women have some lumps or lumpy areas in their breasts all the time, and most breast lumps turn out to be benign (not cancerous). There are a number of possible causes of non-cancerous breast lumps, including normal hormonal changes, a benign breast condition, or an injury.
Call your doctor
Don’t hesitate to call your doctor if you’ve noticed a lump or other breast change that is new. This is especially true for changes that last more than one full menstrual cycle (or one month, for those who don’t menstruate) or seem to get bigger or more prominent in some way. If you menstruate, you may want to wait until after your period to see if the lump or other breast change disappears on its own before calling your primary care provider or gynecologist.
Get it checked out
At an appointment to evaluate a breast lump, your doctor takes a health history and does a physical exam of the breast, and most likely orders breast imaging tests. Ultrasound is often the first or only imaging test used to evaluate a lump in women who are younger than 30 or are pregnant or breastfeeding. Both an ultrasound and a mammogram are typically recommended to evaluate a lump in women who are older than 30 and not pregnant or breastfeeding.
If further testing is needed, your doctor may recommend additional imaging with MRI, a biopsy, or a combination of these tests. Your doctor may also refer you to a breast specialist (typically, a breast surgeon) for further evaluation.
Make sure you get answers
It’s important that your doctor explains what is causing the lump or other breast changes and, if necessary, develops a plan for monitoring it or treating it. If you’re not comfortable with your doctor’s advice, don’t hesitate to get a second opinion.
How to develop breast self-awareness
Make it routine
The more you examine your breasts, the more you can learn about them and the easier it can become for you to tell if something has changed. Examine yourself several days after your period ends, when your breasts are least likely to be swollen and tender. If you are no longer having periods, choose a day that’s easy to remember, such as the first or last day of the month.
Know your breasts
Get to know your breasts’ different “neighborhoods.” The upper, outer area — near your armpit — tends to have the most prominent lumps and bumps. The lower half of your breast can feel like a sandy or pebbly beach. The area under the nipple can feel like a collection of large grains. Another part might feel like a bowl of lumpy oatmeal.
Stay connected with your breasts
Get a new “baseline” after any breast procedure. If you’ve had a breast biopsy, breast surgery, radiation therapy, or other treatments to the breast or chest, you might have scar tissue or breast skin changes. It’s important to get a sense of what your new normal is after healing from a procedure, so you can take that into account when you check your breasts for changes.
Breast and chest self-exams for trans and nonbinary people
Though the research is very limited, transgender men and women who have breast tissue are thought to be at a higher risk for breast cancer than cisgender men. Because of this, they may also consider performing breast or chest self-examinations on a monthly basis. Some medical guidelines recommend against this practice for transgender individuals, however, due to a lack of data to support its efficacy as well as the potential to produce harm (both psychological harm, as well as potential physical harm from an unnecessary biopsy). Transgender men and non-binary people assigned female at birth may experience gender dysphoria when conducting self-examinations.
Crucially, chest masculinization surgery does not remove all breast tissue, so even transgender people who have this surgery are at risk for breast cancer and should consider chest self-examinations and discuss a breast cancer screening imaging plan with their medical team.
Symptoms associated with feminizing hormone therapy — such as breast pain, tenderness, and nodularity — may prompt transgender women and non-binary people assigned male at birth to perform overly frequent breast self-examinations, according to the University of California, San Francisco. Be aware that these symptoms may simply be due to breast growth, and talk to a medical provider if you are concerned.