Dense Breasts
Updated on July 3, 2025
Having dense breasts is usually normal and relatively common. Breast density is not a medical condition itself. It does not usually cause symptoms. For about half of women, mammograms reveal they have breast tissue categorized as dense.
Knowing whether you have dense breasts is important because:
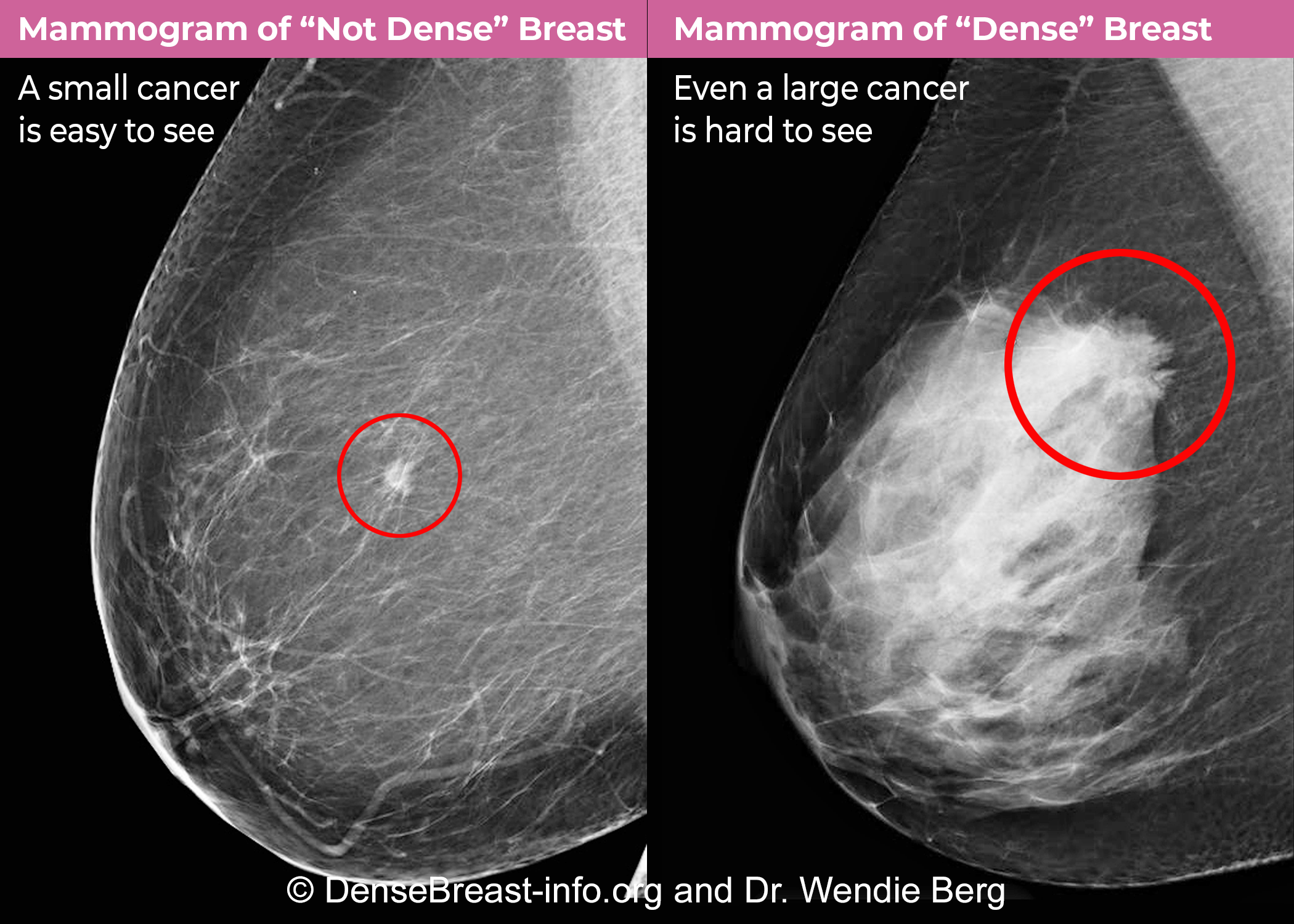
Breast density makes it harder for doctors to see breast cancers on mammograms. This increases the risk that cancers will be missed.
People with dense breasts have a higher risk of developing breast cancer compared to people who don’t have dense breasts. The greater the amount of dense tissue, the higher the risk.
Breast density alone does not predict your risk of breast cancer. It is one piece of the puzzle that affects breast cancer risk and your breast cancer screening plan.
What are dense breasts?
Your breasts are made up of three main types of tissue:
fibrous tissue (supports and holds tissue in place)
glandular tissue (produces milk)
fatty tissue (fills the space between fibrous and glandular tissue)
If you're told you have dense breasts, this means that you have more fibrous and glandular tissue and less fatty tissue than women who don't have dense breasts. That’s why dense breast tissue is also called “fibroglandular tissue” and breast density is also referred to as “fibroglandular density.”
Having dense breasts isn’t something you can control. Breast density is often inherited, but can change over time. Some women are more likely to have dense breasts, such as those who are:
pre-menopausal
post-menopausal and take hormone replacement therapy
lean with low body mass index (BMI)
And some women are less likely to have dense breasts, such as those who:
have gone through menopause
have had children
take anti-estrogen hormonal therapy like tamoxifen, either to lower breast cancer risk or to treat breast cancer; aromatase inhibitors, which are another type of anti-estrogen hormonal therapy, may also decrease breast density, but the impact doesn’t appear to be as substantial.
How is breast density measured?
When you have a mammogram, a radiologist reads the results using the Breast Imaging Reporting and Data System (BI-RADS). This is a standard system for reporting what’s seen on the imaging.
In the BI-RADS report, the radiologist includes a score for breast density on a scale from A through D:
A) Mostly fatty: The breasts are made up of mostly fatty tissue and contain very little fibrous and glandular tissue. About 10% of women have fatty breasts.
B) Scattered fibroglandular densities: The breasts are mostly fatty tissue, but there are a few areas of fibrous and glandular tissue visible on the mammogram. About 40% of women have scattered density.
C) Heterogeneously dense: A mammogram shows many areas of fibrous and glandular tissue. About 40% of women get this result.
D) Extremely dense: The breasts have large amounts of fibrous and glandular tissue. About 10% of women fall into this category.
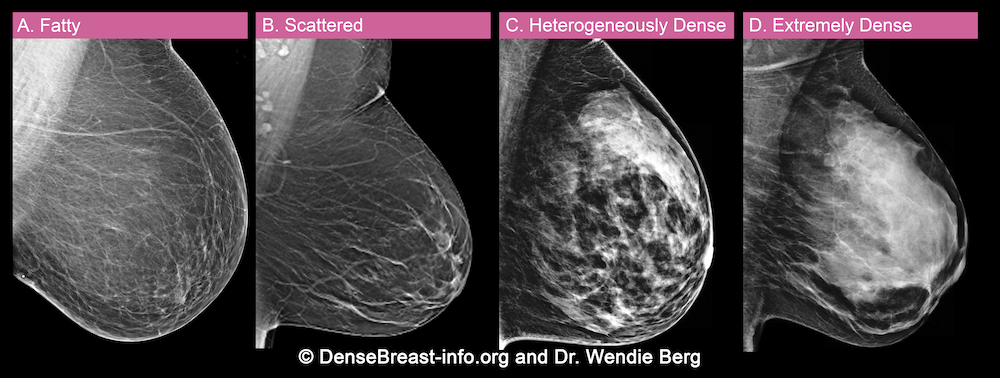
If you’ve had a mammogram and your written report said that you have either “heterogeneously dense” (C) or “extremely dense” (D) breasts according to the BI-RADS scoring system, you have dense breasts.
The radiologist makes the classification, so it often requires a judgment call — and studies suggest that two radiologists may classify the same image differently. 1 For this reason, many breast imaging centers are now using automated software to assist with evaluating breast density.
Why does breast density matter?
If you’ve got dense breasts, it can be harder for radiologists to detect breast cancer when they’re reading your mammogram. This is because cancers typically show up as white spots or masses on a mammogram and dense breast tissue also appears white on a mammogram. Just as it would be hard to spot a polar bear in a blizzard, this makes it hard to tell the difference between normal, healthy tissue and abnormal tissue. Fatty breast tissue appears dark on a mammogram, so it’s easier to see white spots that may represent abnormal tissue.
Mammograms can miss about half of cancers in women with dense breasts. 2 In addition, women with dense breasts are more likely to be diagnosed with breast cancer within a year of receiving a normal mammogram result 3, usually based on symptoms such as a lump or other breast changes.
Besides hiding cancers on mammograms, dense breast tissue itself is associated with a higher risk of breast cancer. Doctors aren’t sure exactly why. Cancers often develop in glandular tissue. The more glandular tissue there is, the greater the risk.
Generally, the more dense breast tissue you have, the higher your risk of breast cancer. It’s important to remember that most women are in the middle two categories of breast density (category B or C). People with extremely dense breast tissue (category D) have double the risk of breast cancer than those who have scattered fibroglandular density (category B).
If you have dense breasts, you and your doctor can talk about this and any other risk factors for breast cancer that you may have. Such risk factors include a family history of breast and other cancers, genetic mutations associated with higher breast cancer risk, and prior radiation treatment to the chest area as an adolescent or young woman.
“Risk in and of itself is multifactorial: it depends on other risk factors you might have in addition to dense breast tissue,” says Maxine Jochelson, MD, director of radiology at the Breast and Imaging Center at Memorial Sloan Kettering Cancer Center in New York City. “If breast density is your only risk factor, that’s one thing, but if there are additional risk factors, that’s different.”
How to find out if you have dense breasts
You can’t identify whether you have dense breasts by a self-exam. Only a mammogram can show whether you have dense breasts.
A U.S. Food and Drug Administration (FDA) rule requires all U.S. mammography facilities to include information on breast density in the written mammogram reports that are sent to you and your doctor. Under the rule, the reports sent to patients must say if the breasts are “dense” or “not dense” (however, they are not required to include the BI-RADS breast density score). The regulations require the use of specific language explaining how breast density can affect the accuracy of a mammogram.
Before the 2023 update, states had different rules about how mammography facilities told women about their breast density. The updated regulations will make breast density reporting consistent throughout the country.
If you live outside the United States, you may or may not be notified about your breast density, depending on the regulations in your country. DenseBreast-info.org is a good resource for finding out what the laws are where you live.
When you read your mammogram report, you may not see the BI-RADS breast density score, but instead see terms such as “mostly fatty” or “scattered fibroglandular density” (meaning your breasts are not dense) or “heterogeneously dense” or “extremely dense” (meaning your breasts are dense).
Breast density asymmetry
Sometimes a mammogram may show what’s called asymmetric density, which means a breast has an area that has greater density than the rest of the breast or has greater density than the same area of the opposite breast. Basically asymmetry means that one side or part of the breast looks different from the rest of the breast tissue or the other side. Asymmetric density is usually only in one breast and not the other. Asymmetries show up as white areas on a mammogram and look different from the normal pattern of breast tissues.
Usually, an asymmetry is benign (not cancerous). But it’s likely your doctor will order more imaging tests to check out the area more carefully.
Cancer screening for women with dense breasts
Know your breast density and make it part of a conversation with your doctor about your annual screening plan.
Research shows that 3D mammograms, also called digital breast tomosynthesis or just tomosynthesis, are more accurate than traditional 2D mammography for women with dense breasts. This can allow the radiologist to see any abnormal cells hidden within the tissue and better characterize their appearance. Check to see if your mammography center offers 3D mammography, and if not, ask your doctor if you can switch to one that does. If this is not an option for you, be sure to keep up to date with your regular annual mammograms.
If you’re among the 10% of women with extremely dense breast tissue on your mammogram, you may want to ask your doctor about whether you can get a second imaging test (called supplemental screening), such as ultrasound or breast MRI, as part of routine screening. Some doctors also may recommend extra screening if you have heterogeneously dense tissue, especially if you have other breast cancer risk factors.
Additionally, if you have dense breasts, consider asking your doctor about getting your breast cancer risk assessed and about extra testing.
“I think if a woman is in the D category — with extremely dense breast tissue — she should know that the mammography alone is very limited in her situation as far as early breast cancer detection,” says Jennifer Harvey, MD, chair of University of Rochester Medical Center Imaging Sciences. “I feel they really should get supplemental screening, as they can benefit from it.”
Extra screening options
Researchers continue to evaluate the best screening options for people with dense breasts. The most common supplemental screening options are:
Ultrasound: Ultrasound is the most widely available supplemental screening option for women with dense breasts. It uses high-frequency sound waves to create images of breast tissue. The images are created as the waves pass through and are reflected by the tissue.
Breast MRI: MRI, or magnetic resonance imaging, is a technology that uses magnets and radio waves to produce detailed 3D images of breast tissue. Before the test, you need to have a contrast solution (dye) injected into your arm through an intravenous line. Cancers take up more of the contrast solution than surrounding normal tissue and become easier to see.
Research is ongoing to determine the value of breast MRI for women with extremely dense breasts. Although breast MRI picks up more breast cancers than ultrasound, it is a much more expensive and involved test, and it may not be available in all areas.
A new version of breast MRI called abbreviated breast MRI (or fast breast MRI) is showing promise as a quicker, less expensive alternative. It takes only about 10 minutes vs. 45 minutes for traditional MRI. It is not yet widely available and is not usually covered by insurance. However, Dr. Harvey notes that some imaging centers are offering this fast breast MRI as a self-pay service. The cost typically ranges from $300 to $500.
Contrast-enhanced digital mammography: Contrast-enhanced mammography (CEM) is just like having a regular mammogram, except for being injected with a contrast solution first (the same type used for CT scans). The contrast helps to highlight any abnormal cancer cells that may be present. CEM is not yet widely available, but studies suggest it may be better than standard mammography combined with ultrasound at finding cancers in dense breasts. A large study in the UK found that CEM can detect three times as many invasive cancers in dense breast tissue as ultrasound. Some studies also suggest that CEM may be just as good as MRI.
Although traditional ultrasound tends to be widely available, the other tests listed might only be available at larger health systems and academic medical centers.
Your doctor can help you figure out the right course of action for seeking supplemental screening — weighing your overall breast cancer risk level, personal preferences, and the availability and cost of additional imaging. For women considered to be at high risk, usually due to a strong family history and/or specific inherited breast cancer-related genetic abnormalities, combined screenings with breast MRI and mammography are recommended starting at age 30.
Insurance coverage for supplemental screening
If you decide to have supplemental screening, your options may depend on what your insurance covers and what’s available in your area. Unlike mammography, which is fully covered by insurance, supplemental imaging often counts toward your deductible and is usually subject to a co-pay, so you may face some out-of-pocket costs.
In the United States, not all insurance companies cover supplemental screening. Coverage depends on your insurance plan and the laws in your state. Some states require insurance coverage for supplemental screening for all women with dense breasts; others limit it to certain groups and certain types of testing.
DenseBreast-info.org maintains a map of U.S. legislation by state that includes information on whether the state has expanded insurance coverage for breast imaging. The website also has information for people in Europe.
You and your doctor should discuss your individual situation, including the amount of dense breast tissue you have and whether you have other breast cancer risk factors. Your doctor’s office may be able to help you find information about supplemental screening options in your area, the cost of supplemental screening, and whether those tests would be covered by your insurance.
Benefits and risks of supplemental screening
Supplemental screening for dense breasts has pros and cons. The main benefit is that adding a second imaging test to your mammogram makes it more likely that your doctor will be able to detect any breast cancer early. It also may give you some peace of mind that you are doing more to find breast cancer early.
The main risk with supplemental screening is that it may lead to unnecessary biopsies, and for some, fear and panic. Imaging tests may identify areas of concern that, after further testing, turn out not to be cancer (known as false positives). The biopsy itself can cause some level of anxiety, as can the uncertainty while waiting for the results. Researchers are still trying to figure out whether the benefits of supplemental screening for all women with dense breasts would outweigh the risks.
“Right now, a lot of it comes down to personal preference,” says Dr. Harvey. “Do you want more testing and possibly undergo a biopsy that wasn’t really necessary, or do you want to risk not finding an early cancer? A lot of it comes down to where an individual’s risk aversion lies.”
Keep in mind that the risk of a “false-positive” callback is the highest the first time you have a specific imaging test. Over time, radiologists will be able to compare your images to see if there are any concerning changes. If you ever switch facilities, it’s important to bring any previous images with you.
Other steps you can take
If you have dense breasts, there are other steps you can take to care for your breast health:
Make sure you have a mammogram every 12 months, and try to go to a center with 3D mammography if possible.
Perform breast self-exams so that you’re aware of any changes in your breasts, which should be reported to your doctor.
Follow the lifestyle recommendations for reducing breast cancer risk, such as:
maintaining a healthy weight
exercising regularly
limiting alcohol consumption
eating nutritious food
not smoking (or quitting if you do smoke)
Visit Risk and Risk Factors for more information.
Sprague BL, Conant EF, Onega T, Garcia MP, Beaber EF, Herschorn SD, et al. Variation in Mammographic Breast Density Assessments Among Radiologists in Clinical Practice: A Multicenter Observational Study. Ann Intern Med. 2016;165(7):457-464. Available at: https://www.acpjournals.org/doi/10.7326/M15-2934
National Institutes of Health Dense Breasts Answers to Commonly Asked Questions. Available at: https://www.cancer.gov/types/breast/breast-changes/dense-breasts#does-having-dense-breast-tissue-affect-a-mammogram
Gordon, P. et al. Breast Density and Risk of Interval Cancers. Canadian Association of Radiologists Journal. 2022;73(1):19-20. Available at: https://journals.sagepub.com/doi/10.1177/08465371211030573